Palliative care report reveals system is failing rural Australians
Despite a rapid increase in the need for palliative care services in Australia, people living in rural areas are still struggling to access end-of-life care.

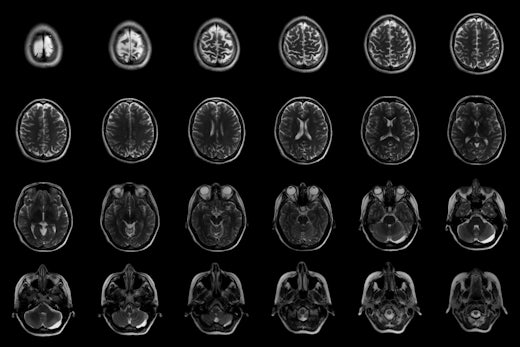
Around 65,000 people were hospitalised for palliative care in 2014/15 (Source: Shutterstock)
A new report released by the Australian Institute of Health and Welfare (AIHW) shows that more people are accessing palliative care services in hospital than ever before.
The report reveals that hospitalisations for palliative care are growing faster than any other incident of hospitalisation, rising by 19 percent between the 2010/11 and 2014/15 financial years. However, the statistics also revealed that access to good palliative care services remain largely dependent on patient location and socioeconomic status.
Palliative Care Australia Chief Executive Officer Liz Callaghan says people living outside of major cities have less access to community-based palliative care options, leaving them more reliant on regional and rural hospitals.
“The national statistics show that regional areas have a higher rate of palliative-care related hospitalisations than major cities,” Says Ms Callaghan.
“We know that 70 percent of Australians would rather die at home than in hospital, but dying at home often requires access to outreach services and community-based support.
“People living outside of major cities don’t get to exercise the same choice about where they die, because they have less access to residential aged care, 24-hour community based services and hospice services – people should be able to access the same level of care regardless of their location.
“It seems capacity to pay also affects choice, with the statistics showing a strong correlation between and palliative care hospitalisations and socioeconomic status.”
Regional hospitals typically employ half as many specialist palliative physicians, per every 100,000 residents, as hospitals in major cities, further compromising the choices of people in those areas.
AIHW Spokesperson Matthew James around 155,600 people died in Australia, with almost half of those dying after being admitted to hospital.
“Of these [people who died in hospital], about 46 percent had been a palliative care patient during their final hospitalisation, up from 37 percent in 2010-11,” says Mr James.
“Although it’s difficult to be definitive about the reasons for this rise, Australia’s growing and ageing population-paired with a rise in chronic and incurable illnesses-has broadened the type of patients requiring palliative care.
“Today’s report shows us that more people are admitted to hospital requiring palliative care services, but we don’t know how many of these people would’ve preferred to have received palliative care services elsewhere.”
Ms Callaghan says the most disadvantaged Australians have double the rate of palliative care-related hospitalisations within the public system compared to people in the highest socioeconomic group, reflecting their reduced capacity to fun private home-based services.
“To put it simply, being able to pay gives you more options, and compounding that, hospices are often located in higher socioeconomic areas of major cities, so people in lower socioeconomic groups don’t have physical or financial access to them,” Ms Callaghan says.
In the 2014/15 financial year there were 65,000 hospitalisations for palliative care. In that same year, nearly half of all patients who died in a hospital as an admitted patient received palliative care of some kind.
In regards to residential aged care facilities, which currently service 192,000 Australians, the report counted only 80 full time-equivalent palliative care nurses working in such facilities across the country.










![The new Aged Care Act exposure draft is slated for release in December of 2023, but advocates hope to see it rolled out on January 1, 2024. [Source: Shutterstock]](https://agedcareguide-assets.imgix.net/news/articles/wp/agedcareact__0811.jpg?fm=pjpg&w=520&format=auto&q=65)












Comments